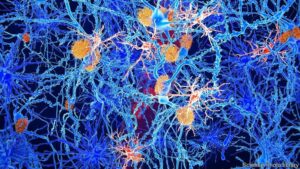
The article talks about an interesting idea: a drug called hydroxychloroquine, once used to treat COVID-19, might help with Alzheimer’s disease because it can reduce inflammation. Dr. Madhav Thambisetty believes this might work, but it’s hard to test because most Alzheimer’s research focuses on a different idea called the amyloid hypothesis. This hypothesis says that certain sticky proteins build up in the brain and cause Alzheimer’s.
For years, scientists have tried to remove these proteins with little success. Recently, some drugs like Leqembi were approved because they can remove these proteins and slightly slow down memory loss, but they are very expensive and have serious side effects.
Some researchers now think other factors might cause Alzheimer’s. Dr. Thambisetty is looking at drugs already approved for other uses, like hydroxychloroquine, to see if they can help with Alzheimer’s. Other scientists are exploring if infections like herpes might be linked to Alzheimer’s. They are getting more funding and attention now.
There are also lifestyle factors, like diet and exercise, that might affect the risk of getting Alzheimer’s. Researchers believe that tackling these factors could help prevent the disease.
Overall, the article suggests that focusing only on the amyloid hypothesis has limited progress and that exploring different ideas might lead to better treatments for Alzheimer’s.
“Ruth Itzhaki, a research scientist at the University of Oxford, stirred curiosity in the 1990s when she shared evidence tying Alzheimer’s to herpesvirus — a scourge spread by oral or genital contact and often resulting in painful infections. For years, powerful promoters of the amyloid hypothesis ignored or dismissed the infection hypothesis for Alzheimer’s, effectively rendering it invisible, Dr. Itzhaki said with exasperation. Research suggests that viruses may hide undetected in organs, including the brain, for years, causing symptoms divergent from the original infection.
But her ideas might finally be catching on. Nearly 5,000 papers have been written about infections and Alzheimer’s since Dr. Itzhaki began her work. National Institutes of Health funding intended in part to examine such links jumped from a few million dollars to nearly $250 million annually in 2023. A clinical trial treating latent herpes among Alzheimer’s patients with an antiviral drug is underway, and results are expected as soon as next year.”